Source link : http://www.bing.com/news/apiclick.aspx?ref=FexRss&aid=&tid=67874bdfe29e4a4aaa5bd943a1bacd9b&url=https%3A%2F%2Fwww.jamaicaobserver.com%2F2025%2F01%2F15%2Ftwo-decades-impact-hic-calls-collaboration-caribbean-healthcare%2F&c=9038609486836694665&mkt=en-us
Author :
Publish date : 2025-01-14 16:05:00
Copyright for syndicated content belongs to the linked Source.
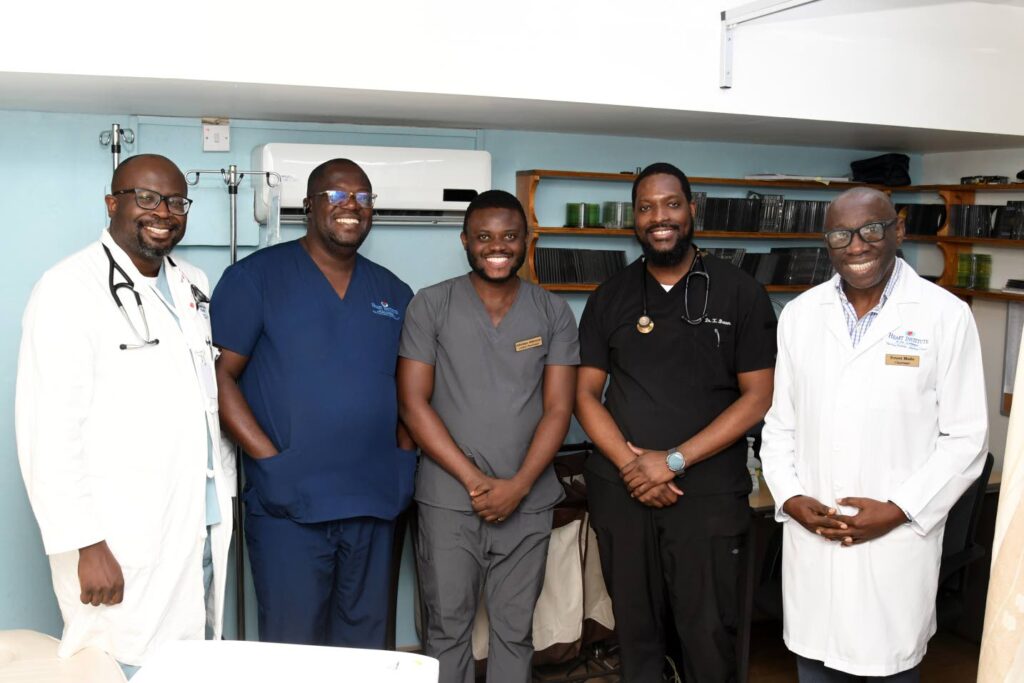
Two decades of impact: HIC calls for collaboration in Caribbean healthcare