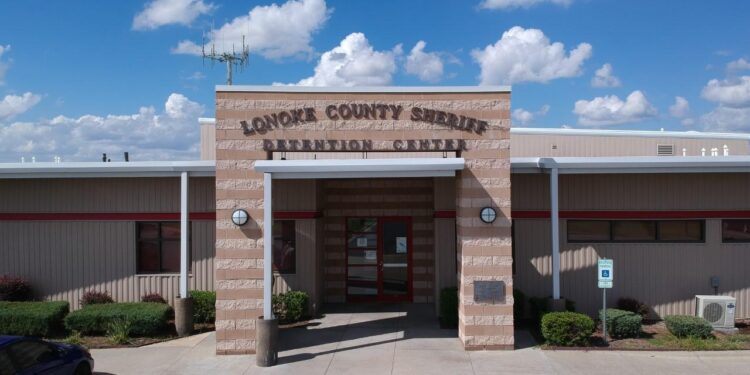
In a troubling echo of historical injustices, recent reports have unveiled a controversial series of ivermectin experiments conducted at an Arkansas jail, drawing sharp criticism and raising alarms about the treatment of imprisoned populations, particularly minorities. The experiments, which purportedly aimed to explore the drug’s efficacy against COVID-19, have ignited a fierce debate over ethical boundaries in medical research and the vulnerability of marginalized groups within the prison system. As advocates demand accountability and transparency, the incidents serve as a stark reminder of the dark legacy of medical exploitation in the United States, where the rights of the incarcerated have often been overlooked. This article delves into the implications of these experiments and the broader context of medical ethics, historical abuses, and the ongoing fight for justice.
Arkansas Jail’s Ivermectin Trials Expose Historical Patterns of Medical Exploitation in Minority Communities
The recent revelation of ivermectin trials conducted on inmates at an Arkansas jail has reignited discussions surrounding the long-standing patterns of medical exploitation faced by minority communities, particularly those in carceral settings. Historical instances of unethical experimentation, heavily documented in the contexts of both race and incarceration, illustrate a disturbing legacy that can be traced back to notorious cases like the Tuskegee Syphilis Study. In this latest episode, the administration of unproven treatments under the guise of medical research raises alarms about consent, transparency, and the true motivations behind such trials.
Critics argue that this situation exemplifies a broader trend of institutional neglect and systemic racism, where marginalized populations are disproportionately subjected to dubious medical practices. Key points of concern include:
- Informed Consent: Questions over whether inmates fully understood the implications of participating in the trials.
- Disparate Impact: How such studies primarily target communities already facing health disparities.
- Historical Precedence: The shadows of past abuses affecting current trust in the healthcare system among minorities.
Furthermore, transparency in these experiments remains critically lacking. Below is a summary of significant historical abuses that echo in the current conversation:
| Event | Year | Community Affected |
|---|---|---|
| Tuskegee Syphilis Study | 1932-1972 | African American Men |
| Willowbrook State School | 1950s-1970s | Intellectually Disabled |
| MKUltra | 1950s-1970s | Various Populations |
Calls for Transparency and Ethical Oversight Over Medical Practices in Correctional Facilities
The recent investigation into ivermectin trials conducted on incarcerated individuals in Arkansas has ignited a pressing dialogue surrounding ethical standards and transparency in medical practices within correctional facilities. Such incidents not only raise alarms but also echo a dark history of medical experimentation on marginalized groups, particularly minorities. The ethical implications are staggering, prompting advocates to emphasize the necessity for a comprehensive framework that ensures informed consent, equitable treatment, and accountability for all medical interventions in jails and prisons.
To address these concerns, experts suggest implementing a robust system of oversight that includes:
- Independent Audits: Regular reviews by external bodies to monitor compliance with ethical standards.
- Informed Consent Protocols: Clear and comprehensible processes for inmates to understand the treatments they undergo.
- Training for Medical Staff: Continuous education on human rights and ethical medical practices tailored to correctional environments.
- Transparent Reporting Mechanisms: Channels for inmates and staff to report unethical practices without fear of retaliation.
A proposed framework for establishing oversight includes a dedicated body that would regulate medical practices in correctional facilities. This body would not only focus on preventing abuses but also ensure that interventions are scientifically validated and respectfully administered. The table below outlines essential aspects of this proposed oversight structure:
| Oversight Aspect | Description |
|---|---|
| Regulatory Body | Establish an independent committee of medical professionals, ethicists, and community representatives. |
| Regular Evaluations | Conduct bi-annual assessments of medical procedures and outcomes within correctional facilities. |
| Public Accountability | Release annual reports detailing practices, compliance levels, and any incidents of malpractice. |
Addressing Systemic Inequities: Recommendations for Reforming Health Care Standards in Prisons
The recent revelations regarding the administration of ivermectin in Arkansas prisons have highlighted the pressing need for reform in the health care standards within correctional facilities. Systemic inequities have long plagued the prison health care system, disproportionately affecting minority populations who often face inadequate medical attention and unethical experimentation. To reform these standards, it is essential to adopt a framework that prioritizes transparency, accountability, and informed consent. Essential steps include:
- Implementing rigorous oversight mechanisms to monitor prisoner health care practices.
- Ensuring that all medical treatments are evidence-based and ethically administered.
- Creating robust channels for prisoners to report health care grievances without fear of retaliation.
- Integrating culturally competent health care professionals into prison systems to address the unique needs of diverse populations.
Additionally, collaboration with independent health organizations can facilitate systemic change by providing resources and expertise to implement best practices. Establishing equity-focused training programs for staff and medical providers will enhance their understanding of the specific challenges faced by marginalized groups. A practical approach can be seen in the following table comparing current practices and proposed reforms:
| Current Practices | Proposed Reforms |
|---|---|
| Limited access to medical care | Guaranteed access to full spectrum health services |
| Lack of informed consent | Mandatory explanations of treatment options |
| Minimal oversight of health services | Regular audits by independent bodies |
To Wrap It Up
In reflecting on the troubling reports surrounding the Arkansas jail’s ivermectin experiments, we are reminded of the historical injustices faced by marginalized communities, particularly within the realm of medical ethics. The use of prisoners in drug trials without informed consent is a stark reminder of past abuses that echo through the corridors of history, raising urgent questions about the protection and autonomy of vulnerable populations. As scrutiny mounts over these practices, it is essential for policymakers, medical professionals, and society at large to confront this troubling legacy and ensure that such violations do not recur in any form. The call for accountability and reform is louder than ever, urging a collective commitment to uphold the dignity and rights of all individuals, regardless of their circumstances. As we move forward, it is crucial that the lessons of the past guide our actions, paving the way for a more just and ethical approach to healthcare for everyone.